Just 2% of Australian men report painful sex compared with 20% of women. Yet, sexual difficulties in women remain overlooked, underreported and therefore go unassisted.
We often hear of men struggling to get it ‘up’ but rarely hear about women who can’t get it ‘in’, while sexual difficulties arise for both men and women, the disparity in attention and awareness is stark. Male sexual problems like erectile dysfunction exist in the public consciousness and receive pharmaceutical companies’ assistance with medications such as the ‘little blue pill’ – Viagra readily available. Comparatively, female sexual difficulties are often unrecognised and ignored.
For some women, the experience of pain during sex is temporary and easily attributed to causes like a UTI, thrush or insufficient foreplay. But for others, pain can be protracted, anxiety-inducing or lead to a total inability to have sex.
An Australian study found that 20% of women experienced pain during sex for at least one month during the year, compared with just 2% of men.
Vaginismus is one of the most common conditions leading to painful sex in women. One woman described her experience of vaginismus as ‘your vagina cockblocking itself’. Another like ‘hitting a brick wall’ and ‘your body at odds with your mind’.
Emily Vernem in an article for Mamamia described feeling ‘immense rage and jealousy’ during conversations with her friends about casual sex. For her friends, casual sex was a regular, naturally occurring and fun experience. But for Emily, it was one she had to mentally build herself up for and prepare months in advance; noting the exasperating disconnect between her sexual encounters and those of her peers. Emily confessed she had believed all women found penetrative sex incredibly painful and thought that everyone was just pretending to enjoy it.
Many women, especially young women, feel this sense of frustration because while it appears as though everyone else is thoughtlessly enjoying painless sex, for them, the experience is stress-inducing, awkward, and at its most severe, incredibly painful. The secret suffering and self-blame that has been revealed since greater awareness and research has been conducted demonstrates just how important it is to speak with each other and trusted health care professionals about sex.
A study conducted in 2019 found that 57% of female patients who attended the Sexual Medicine and Therapy Clinic (Monash Health) attended due to painful sex, and 60% of them had vaginismus. Almost half of these women experienced this for 5+ years, and 1-in-5 of those women experienced it for 10+ years.
Vaginismus is the involuntary contracting or tightness of the muscles surrounding the vagina that make sex painful or impossible. Women report a ‘burning pain’ and tightness that you cannot relieve yourself. Vaginismus is caused by spasms or involuntary contraction of the pelvic floor muscles. The pelvic floor is too strong and the muscles too tight, which results in an inability to relax the muscles when you are trying to have sex or insert something into the vagina.
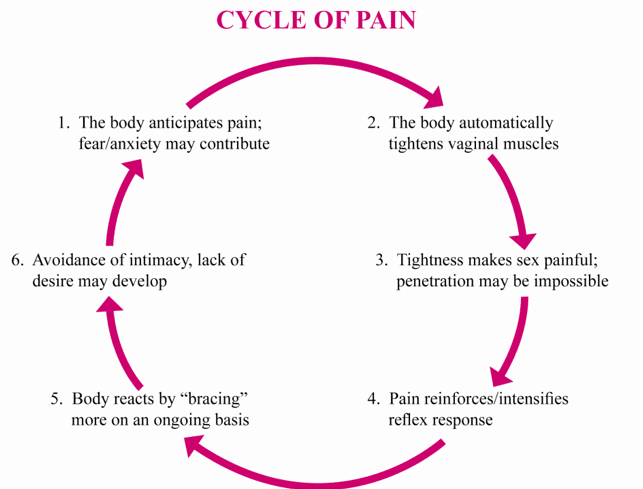
Vaginismus is a unique condition that can have either physical or non-physical causes, or in some cases, no apparent cause at all. Often the physical becomes psychological and vice versa. Anxiety leads the body to develop muscle memory that conditions a response against penetration.
Women who hold tension in their pelvic floor can experience primary or secondary vaginismus.
Primary vaginismus occurs from the first time anything is attempted to be inserted into the vagina; a tampon, a finger, or having sex for the first time. The major causes for primary vaginismus can include fear around sex, not being ready, and feeling pressured. For others, it may be the result of cultural or religious pressure to remain celibate until marriage.
Secondary vaginismus referred to when sex was fine, to begin with, but something changed that then led to pain. Some of the reasons this can occurs are childbirth, endometriosis, trauma, or having the kind of sex you don’t enjoy that may start as a bit of discomfort but over time develops into aversion.
While this can be an extraordinarily infuriating and uncomfortable experience, it’s important to consider that treatment can resolve vaginismus. The type of treatment required is dependent on the cause of the condition and will be tailored specifically to your personal goals. Commonly, counselling and physiotherapy are needed to address both the physical and the psychological factors at play.
Counselling aims to identify and work on the negative perceptions involving body image and sex and can help to manage the pain, fear and anxiety. Physiotherapy focuses on retraining the pelvic floor muscles and includes desensitisation techniques. This method helps regain conscious control of the pelvic floor muscles and is generally achieved through dilators and exercises.

Sex and relationship therapist, Lisa Torney, explains that women have been socialised to prioritise male sexual pleasure, forcing female pleasure to take a backseat for centuries.
Alongside the lack of adequate sexual education, young women are often told that their first experience of sexual intercourse will hurt, which Torney points out is often how vaginismus for many women begins.
Treatment often centres on a reframing of the individual’s feelings on sex, emphasising it should be enjoyable and that often feelings about sex operate cyclically. Feeling comfortable leads to feeling aroused, ensuring greater comfort and making sex both more pleasant and pleasurable.
When discussing sex and our bodies, the conversation has to shift from expectations of dissatisfaction or the limits of what we can endure to one of positivity, empowerment and pleasure. Vaginismus is a common condition and one that we should not suffer in silence. Sex should not be painful, using a tampon should not cause distress and pap smears should only be uncomfortable, never excruciating.







