Increasingly, research is demonstrating that when combined with psychotherapy, psychedelic drugs are a safe and effective treatment option where traditional methods have failed.
After decades of stigmatisation, psychedelics are again being used as an adjunct to psychotherapy, or ‘talk-therapy’. Depression, anxiety, obsessive-compulsive disorder (OCD), eating disorders, post-traumatic stress disorder (PTSD), and addiction are being successfully treated with psychedelics like psilocybin (magic mushrooms) and MDMA (ecstasy) where prescription medications have failed.
With rates of mental illness in Australia increasing, the expansion of available treatment options is welcome news to many.
With rates of mental illness in Australia increasing, the expansion of available treatment options is welcome news to many. The Australian Bureau of Statistics’ (ABS) National Health Survey for 2017-18 reported that 20% of Australians had a mental or behavioural condition, up from 17.5% reported in 2014-15. Social restrictions brought about by onset of the COVID-19 pandemic have further negatively impacted mental health in this country.
Enter Mind Medicine Australia (MMA), a non-profit organisation and peak body that has, since 2019, been championing the benefits of psychedelic-assisted therapy.
Co-founder Tania de Jong’s interest in the therapeutic use of psychedelics was piqued when she read a 2015 New Yorker article by American author and journalist, Michael Pollan, about the use of psilocybin-assisted therapy on cancer patients.

Tania says, “These medicines have been with humanity since the beginning of human civilisation. You can see them in the archaeology of ancient Rome and Greece and South American cultures, many Indigenous cultures. They continue to use these medicines for healing, for raising of consciousness in many communities around the world.”
Determined to conduct her own research, Tania sought out available psychedelic drug trials in Europe. Finding none, she and her husband, Peter Hunt, travelled to the Netherlands where magic mushrooms are legal for personal use. After ingesting Syrian rue, which enhances and prolongs the effects of psychedelics, she and Peter took magic mushrooms. The pair were forever changed.
Our sense of oneness, of connection with self, with others, with the planet, was so profound … Now I recognise that everything is part of me and I’m part of everything, that we are all connected.
“Our sense of oneness, of connection with self, with others, with the planet, was so profound,” Tania says of the experience. “Nothing looks the same to me anymore. Now I recognise that everything is part of me and I’m part of everything, that we are all connected.”
Reminded of the work of Johann Hari, who posits that humans’ need for connection with others has to be met to counter the effects of mental illness, Tania’s personal experience solidified her belief that psychedelic drugs like psilocybin and MDMA, commonly known as ecstasy, could help people reconnect with themselves and others.
Consequently, Tania and Peter founded MMA, drawing upon the expertise of doctors, patients, academics, government, and regulatory bodies to produce evidence-based support for the clinical use of psychedelic-assisted therapy.
Psychedelic-assisted therapy, the use of psychotherapy alongside the ingestion of a psychedelic drug, had previously proven to be very effective. Between 1954 and 1960, English psychiatrist Humphry Osmond – the man who coined the term ‘psychedelic’ from the Greek for ‘mind-manifesting’ – teamed up with Canadian biochemist Abram Hoffer to administer LSD to treatment-resistant alcoholics. Of the 2,000 patients treated, 40% to 45% had not relapsed after one year.
At around the same time, British psychiatrist Ronald Sandison was achieving similar results using LSD-assisted psychotherapy. Between 1950 and 1965, around 40,000 patients had been prescribed LSD therapy to treat a range of mental illnesses.
However, in the late 1960s, after LSD made its way onto American streets and its use quickly spread to the UK and Europe, research into psychedelics was halted. Considered a drug of abuse that epitomised the counterculture of the time, then-President Nixon eventually criminalised the use, sale, possession and manufacture of LSD and other drugs as part of his war on drugs. The UK and Europe followed suit.
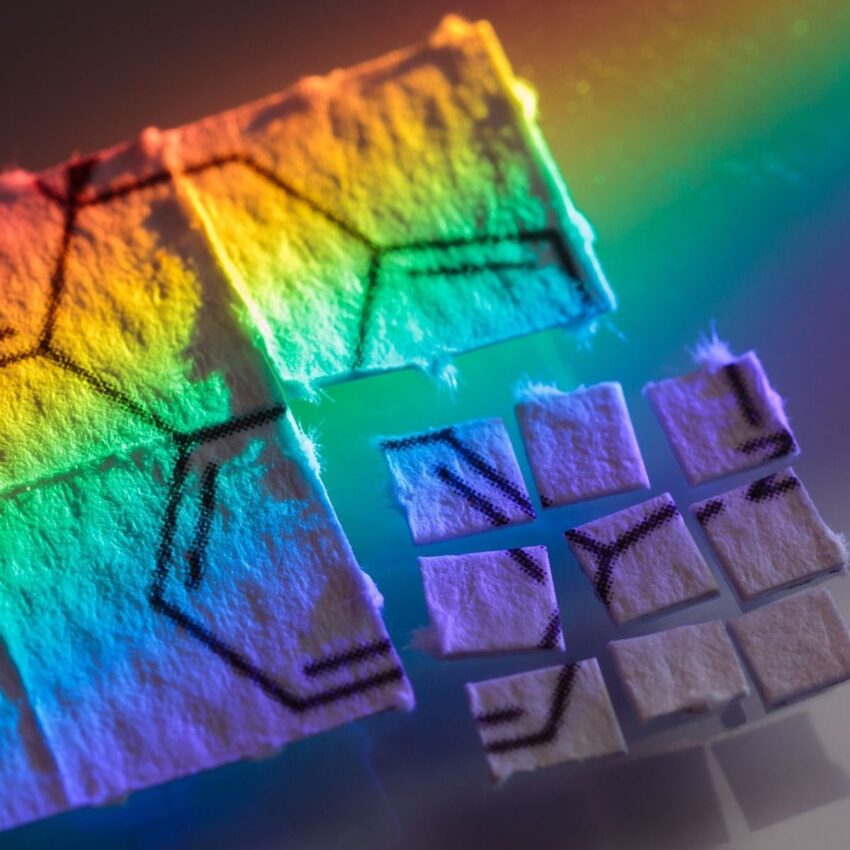
The past decade has seen a return to psychedelic-assisted therapy, in part because the way these drugs work is better understood. Research has shown that psilocybin disrupts default connections in the brain, creating a state of neuroplasticity – the ability of the brain to reorganise itself – which makes an individual more susceptible and receptive to psychotherapy. Whereas MDMA is known to produce empathy, well-being, insightfulness, compassion for oneself and others, and, importantly, an ability to access to emotionally intense material.

As Tania explains, psychedelic-assisted therapy “provides this incredible opportunity for a patient to become an agent for their own healing, to start to feel empowered for their own healing rather than taking a daily pharmaceutical psychiatric medication with its multiple side effects that mostly, at best, tends to numb out the highs and lows of life.”
Psychedelic-assisted therapy provides this incredible opportunity for a patient to become an agent for their own healing, to start to feel empowered.
While one person’s psychedelic experience is never the same as another’s, the process of psychedelic-assisted therapy has been standardised and is made up of three phases:
- Preparation, or the development of a therapeutic relationship between patient and therapist over a series of pre-treatment sessions.
- The acute psychedelic experience, which typically lasts about eight hours and is usually attended by two therapists who support the patient as needed. Here, ‘set’ (the patient’s mindset) and ‘setting’ (the physical environment) are paramount.
- Integration.
Integration is crucial to the success of psychedelic-assisted therapy, providing an opportunity for the patient to assign meaning to their psychedelic experience. Integration allows traumatic experiences to be fully explored, exposing valuable insights. As Tania explains, the process of integration creates “an incredible therapeutic window for a trained therapist to come and work with that patient to help them to come to terms with whatever traumas are holding them back and keeping them stuck in the past.”

The US has been at the forefront of research into psychedelic-assisted therapies. In 2010, MDMA-assisted psychotherapy was administered to patients with treatment-resistant PTSD, resulting in an immediate and significant reduction in symptoms that was still present after three-and-a-half years.
Psilocybin-assisted psychotherapy was then trialled on patients with treatment-resistant depression. After three months, 42% of patients remained in complete remission. When trialled on patients with depression and anxiety after a diagnosis of life-threatening cancer, 60 to 80% of participants had significantly reduced depression and anxiety after six months. A subsequent larger clinical trial involving end-stage cancer patients showed that about 80% of participants had a substantial decrease in depression and anxiety after six months.
Psilocybin has also been used with good effect in the treatment of tobacco and alcohol use disorders.
The Multidisciplinary Association for Psychedelic Studies (MAPS) has been behind much of this research. The organisation is currently sponsoring FDA research into MDMA-assisted therapy for the treatment of severe PTSD which is showing a significant improvement in symptoms with no major safety issues.
Based on the results of trials like these, the US Food and Drug Administration (FDA) has designated MDMA and psilocybin ‘breakthrough therapies’ in the treatment of mental illness.
This is the first time that MDMA will be administered to Australian patients with treatment-resistant PTSD.
Now MMA is following in MAPS’ footsteps. In May 2021, MMA partnered with drug developer Emyria to launch a clinical trial modelled on MAPS’ MDMA-assisted psychotherapy trial. This is the first time that MDMA will be administered to Australian patients with treatment-resistant PTSD. MMA has also petitioned the Therapeutic Goods Administration (TGA) to down-schedule psilocybin and MDMA from classification as prohibited (Schedule 9) drugs to controlled, Schedule 8, drugs.
In August this year, the TGA appointed an independent panel to review the role of psychedelics in the treatment of mental illness before making their final decision in relation to down-scheduling.
Currently, medical practitioners can apply to the TGA for access to an ‘unapproved drug’ under Category B of the Special Access Scheme, provided they can provide clinical justification for its use. Tania states that, so far, there have been over 40 approvals for the use of psilocybin- and MDMA-assisted psychotherapy under this Scheme. But the process is lengthy, and approval is not guaranteed.
While the TGA’s independent assessment of the therapeutic benefit of psychedelics is encouraging, there is still resistance to their use. The Royal Australian and New Zealand College of Psychiatrists (RANZCP) opposed the proposed down-scheduling, calling for further research to assess the safety and efficacy of psychedelics despite the promising results already produced by worldwide clinical trials.

Interestingly, in 2019 the Journal of Psychopharmacology found the most harmful drug used by Australians was alcohol, followed by cigarettes, crystal methamphetamine, cannabis, heroin and pharmaceutical opioids. Psychedelics did not rate a mention.
Resistance to the therapeutic use of psychedelics is underpinned by society’s exposure to decades of anti-drug rhetoric, a consequence of the failed war on drugs.
Resistance to the therapeutic use of psychedelics is underpinned by society’s exposure to decades of anti-drug rhetoric, a consequence of the failed war on drugs. Consequently, the development of new treatments for mental illness has stalled. It is only when the paradigm shifts that the benefits of psychedelic-assisted therapies will be fully realised.
MMA intends to create that paradigm shift in Australia. Tania is urging medical and psychiatric communities, government agencies, and the public to focus on the available research data and “stop with all the stigma and prejudice of the past which has held us back for such an enormously long time.”
If you’d like to learn more about Tania de Jong’s work and Mind Medicine Australia, watch our exclusive interview with her below.







